Items filtered by date: March 2022
Dealing With Peripheral Artery Disease
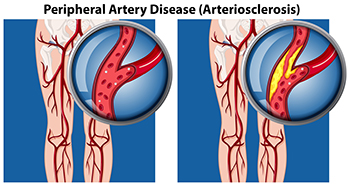
When blood flow to the extremities slows, particularly to the feet, it most likely is caused by a blockage of the arteries. This condition, called peripheral arterial disease (PAD), is very common. Smoking, obesity, poor eating habits, and being sedentary are major factors in the development of PAD. Other maladies, such as diabetes and hypertension, can further cause the blood vessels to narrow. Symptoms of PAD include pain and cramping in the legs and feet when walking, numbness, sores that don’t heal, and foot pain when at rest. Some life changes can help reduce the symptoms, such as lowering fats and cholesterol in your diet, moving around more, reducing stress, stopping smoking, and lowering your blood pressure. If you develop sores on your feet and ankles that refuse to heal, and are experiencing other PAD symptoms, it is a good idea to make an appointment with a podiatrist for an examination and ongoing treatment plan.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our podiatrists from Advanced Ankle & Foot Surgeons. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in O'Fallon, and New Baden, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Why Pain From Plantar Fasciitis Is Worse in the Morning
Plantar fasciitis will affect 1 in 10 people, mostly between the ages of 40-60, or younger if they are runners, athletes or dancers. The plantar fascia is the web-like fibrous tissue connecting the heel bone with the toes on the sole of the feet. Stress, micro-tears or other damage to the plantar fascia can cause it to become inflamed, which results in plantar fasciitis. This inflammation, in turn, causes the plantar fascia to tighten during periods of rest or inactivity and typically produces a sharp, stabbing pain towards the middle of heel, where the plantar fascia attaches to it. Initially, once activity is resumed (after waking in the morning, for example), and the plantar fascia begins to stretch, the pain may subside, but will reoccur later in the day. Contributing factors to plantar fasciitis include obesity, foot structure disorders such as flat feet or high arches, having to stand for prolonged periods, and participating in sporting activities with repetitive stress on the plantar fascia (i.e., running and jogging). If you have heel pain, it is a good idea to make an appointment with a podiatrist who can determine if plantar fasciitis is the cause and create a treatment plan to reduce your pain and help repair the plantar fascia.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Advanced Ankle & Foot Surgeons. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in O'Fallon, and New Baden, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Healing of a Broken Ankle
 Broken ankles are usually caused by the ankle turning, twisting, or rolling while walking, running, or participating in sports. An ankle can also break from repetitive stress (stress fracture) or high-impact trauma to the ankle, like a fall or an auto accident (traumatic ankle fracture). Some ankle fractures can occur where bones break but remain in correct alignment, while in other instances, portions of the bone become separated or misaligned. Pain and swelling will typically occur in the ankle area and parts of the foot, and might radiate up to the knee. Putting weight on the affected ankle can make all symptoms worse. Different types of fractures require different treatment based on alignment and stability of the ankle. X-rays, a CT scan or an MRI may be needed to determine the extent of the injury. Seeing a podiatrist will help determine which type of fracture has been sustained and the proper course of treatment to help preserve the ankle joint for life.
Broken ankles are usually caused by the ankle turning, twisting, or rolling while walking, running, or participating in sports. An ankle can also break from repetitive stress (stress fracture) or high-impact trauma to the ankle, like a fall or an auto accident (traumatic ankle fracture). Some ankle fractures can occur where bones break but remain in correct alignment, while in other instances, portions of the bone become separated or misaligned. Pain and swelling will typically occur in the ankle area and parts of the foot, and might radiate up to the knee. Putting weight on the affected ankle can make all symptoms worse. Different types of fractures require different treatment based on alignment and stability of the ankle. X-rays, a CT scan or an MRI may be needed to determine the extent of the injury. Seeing a podiatrist will help determine which type of fracture has been sustained and the proper course of treatment to help preserve the ankle joint for life.
Broken ankles need immediate treatment. If you are seeking treatment, contact one of our podiatrists from Advanced Ankle & Foot Surgeons. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Ankles
A broken ankle is experienced when a person fractures their tibia or fibula in the lower leg and ankle area. Both of these bones are attached at the bottom of the leg and combine to form what we know to be our ankle.
When a physician is referring to a break of the ankle, he or she is usually referring to a break in the area where the tibia and fibula are joined to create our ankle joint. Ankles are more prone to fractures because the ankle is an area that suffers a lot of pressure and stress. There are some obvious signs when a person experiences a fractured ankle, and the following symptoms may be present.
Symptoms of a Fractured Ankle
- Excessive pain when the area is touched or when any pressure is placed on the ankle
- Swelling around the area
- Bruising of the area
- Area appears to be deformed
If you suspect an ankle fracture, it is recommended to seek treatment as soon as possible. The sooner you have your podiatrist diagnose the fracture, the quicker you’ll be on the way towards recovery.
If you have any questions, please feel free to contact our office located in O'Fallon, and New Baden, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Reminder: When Was the Last Time...?
When Gout Flares up in the Big Toe Joint
If your big toe joint suddenly gets hot, red, swollen, and very painful, you could be having a gout flare. Gout is an arthritic condition that develops when excessive amounts of uric acid in the body cluster and crystallize on joints—most commonly the big toe joint. Symptoms from a gout flare can last for days or weeks and then completely disappear until the next flare occurs. You may be more at risk of developing gout if you have a family history of it, or if you are male, obese, drink alcohol, eat a lot of purine-rich red meat and seafood, or have certain health conditions like diabetes, kidney issues, hypertension, congestive heart failure, diabetes and more. If you believe you may have gout, it's a good idea to make an appointment with a podiatrist who can diagnose your condition through an exam and various tests, and help relieve your pain. In severe cases, where large deposits of gout form and normal pain relief methods do not provide relief (or there is joint dysfunction), surgery may be necessary.
Gout is a painful condition that can be treated. If you are seeking treatment, contact one of our podiatrists from Advanced Ankle & Foot Surgeons. Our doctors will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our office located in O'Fallon, and New Baden, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Why Diabetes and Podiatry Go Together
 There are a variety of complications to the feet that diabetes can cause, and some of them can even lead to amputation. These problems occur because diabetic patients are prone to losing the sensation in their feet, making it difficult to notice problems in their early stages. Diabetes can also cause poor blood flow in the feet, which ultimately leads to both numbness and a slower healing process for wounds. This is why it is important for diabetic patients to develop a foot care routine that includes checking the feet every day for wounds and sores, keeping the feet clean, keeping the skin soft and smooth, and finding properly fitting footwear. Regular checkups with a podiatrist are also suggested for diabetic patients. Anyone with diabetes who has further questions or concerns shouldn’t hesitate to consult with a podiatrist near them.
There are a variety of complications to the feet that diabetes can cause, and some of them can even lead to amputation. These problems occur because diabetic patients are prone to losing the sensation in their feet, making it difficult to notice problems in their early stages. Diabetes can also cause poor blood flow in the feet, which ultimately leads to both numbness and a slower healing process for wounds. This is why it is important for diabetic patients to develop a foot care routine that includes checking the feet every day for wounds and sores, keeping the feet clean, keeping the skin soft and smooth, and finding properly fitting footwear. Regular checkups with a podiatrist are also suggested for diabetic patients. Anyone with diabetes who has further questions or concerns shouldn’t hesitate to consult with a podiatrist near them.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Advanced Ankle & Foot Surgeons. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in O'Fallon, and New Baden, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.