How Podiatrists Help Patients Manage Chronic Foot Pain
 Podiatrists play an important role in managing chronic foot pain. Podiatrists can diagnose the underlying causes of the pain and also implement targeted treatment plans. These doctors have the specialized knowledge it takes to pinpoint the source of the foot pain, whether it be caused by structural issues, biomechanical abnormalities, or conditions such as arthritis or neuropathy. They may perform assessments and diagnostic tests to find the answers patients in pain are looking for. Based on the diagnosis, podiatrists may recommend a variety of interventions to ease pain, including custom orthotic inserts to correct foot alignment, stretches to strengthen muscles and improve flexibility, or corticosteroid injections to reduce inflammation and alleviate pain. Podiatrists can also provide guidance on proper footwear selection and offer lifestyle modifications to minimize stress on the feet. By addressing the root cause of chronic foot pain and tailoring treatment plans to individual needs, podiatrists empower patients to find relief and regain mobility, which can greatly enhance quality of life. If you have persisting foot pain, it is suggested that you visit a podiatrist who can diagnose you and provide a personalized treatment plan.
Podiatrists play an important role in managing chronic foot pain. Podiatrists can diagnose the underlying causes of the pain and also implement targeted treatment plans. These doctors have the specialized knowledge it takes to pinpoint the source of the foot pain, whether it be caused by structural issues, biomechanical abnormalities, or conditions such as arthritis or neuropathy. They may perform assessments and diagnostic tests to find the answers patients in pain are looking for. Based on the diagnosis, podiatrists may recommend a variety of interventions to ease pain, including custom orthotic inserts to correct foot alignment, stretches to strengthen muscles and improve flexibility, or corticosteroid injections to reduce inflammation and alleviate pain. Podiatrists can also provide guidance on proper footwear selection and offer lifestyle modifications to minimize stress on the feet. By addressing the root cause of chronic foot pain and tailoring treatment plans to individual needs, podiatrists empower patients to find relief and regain mobility, which can greatly enhance quality of life. If you have persisting foot pain, it is suggested that you visit a podiatrist who can diagnose you and provide a personalized treatment plan.
If you are experiencing pain in the feet or ankles, don’t join the stubborn majority refusing treatment. Feel free to contact one of our podiatrists from Advanced Ankle & Foot Surgeons. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
Someone would seek the care of a podiatrist if they have suffered a foot injury or have common foot ailments such as heal spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, etc.
Podiatric Treatment
A podiatrist will treat the problematic areas of the feet, ankle or lower leg by prescribing the following:
- Physical therapy
- Drugs
- Orthotic inserts or soles
- Surgery on lower extremity fractures
A common podiatric procedure a podiatrist will use is a scanner or force plate which will allow the podiatrist to know the designs of orthotics. Patients are then told to follow a series of tasks to complete the treatment. The computer will scan the foot a see which areas show weight distribution and pressure points. The podiatrist will read the analysis and then determine which treatment plans are available.
If you have any questions please feel free to contact our office located in O'Fallon, and New Baden, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
The branch of medicine that is focused on the treatment, diagnosis, and study of disorders of the lower leg, ankle and foot is referred to as podiatry. Because people often spend a great deal of their time on their feet, many problems in this area can occur. A person seeks help from the field of podiatry when they need treatment for heel spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, infections, and problems with the foot that are related to diabetes and additional diseases.
To treat problems of the foot, ankle or lower leg, a podiatrist may prescribe physical therapy, drugs, perform surgery, or set fractures. Individuals may also be recommended to wear corrective shoe inserts, custom-made shoes, plaster casts and strappings in order to correct deformities.
When trying to gather information on a patient problem, a scanner or force plate may be used in order to design orthotics. During this procedure, patients are told to walk across a plate that is connected to a computer; the computer then takes a scan of the foot and indicates weight distribution and pressure points. The computer readouts will give the podiatrist information to help them determine the correct treatment plans.
Diagnosis is also provided through laboratory tests and x-rays. Through the foot, the first signs of serious problems such as heart disease, diabetes and arthritis can show up. For example, individuals that have diabetes may frequently have problems such as infections and foot ulcers because they experience poor circulation in the foot area. A podiatrist can then have consultations with patients when symptoms arise. Referrals will then be made to specialists that handle the greater health problems.
Some podiatrists have their own independent, private practices or clinics where they have a small staff and administrative personnel. Many podiatrists work within group practices. They usually spend time performing surgery in ambulatory surgical centers or hospitals, or visit patients in nursing homes. Podiatrists typically spend between 30 to 60 hours of week working. Some podiatrists specialize in public health, orthopedics, surgery, or primary care. Other fields include specialties in geriatrics, dermatology, pediatrics, diabetic foot care and sports medicine.
Some podiatrist specialists complete extra training in the area of foot and ankle reconstruction that results from the effects of physical trauma or diabetes. There are also surgeons that perform surgery of a cosmetic nature to correct bunions and hammertoes.
Finding the Right Shoe Size With Consideration for Orthotics Fit

Navigating shoe sizing can be a perplexing endeavor, compounded by variations in size between brands and styles. To ascertain the right shoe size, inspecting your existing footwear collection is beneficial, making note of sizes across different brands and styles. This knowledge proves invaluable in choosing the appropriate size for your desired comfort. When shopping for shoes, emphasize aligning the width, flex point, and instep with your foot to ensure a proper fit. Additionally, be mindful of how the choice of materials can affect stretching over time. Context plays a significant role; consider the intended use of the shoe and any foot-related health concerns. Comfort is most important for the perfect fit. Experimenting with at least three sizes is advisable to identify the most comfortable. Be aware that sizing discrepancies can even exist within the same brand. Above all, avoid forcing a fit that may result in discomfort and potential injury. Additionally, ensure that any orthotics you use fit seamlessly with your chosen shoe size for optimal foot support and comfort. If you are having trouble getting the right shoe size for your needs, including fitting orthotics into shoes, it is suggested that you consult a podiatrist who can guide you in this quest.
If you are having discomfort in your feet and would like to try orthotics, contact one of our podiatrists from Advanced Ankle & Foot Surgeons. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in O'Fallon, and New Baden, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Foot Orthotics for Athletes
Ankle foot orthotics are shoe inserts that offer support to control the placement and movement of the ankle, correct deformities, and compensate for weakness. These inserts are used to stabilize the foot and ankle and provide toe clearance during the swing phase of gate.
Athletes often suffer foot problems because their feet are not being supported within the shoe. Ankle and foot orthotics are custom made inserts that alleviate stress on the foot. However custom orthotics should be prescribed by a podiatrist who specializes in customized footwear and orthotics design. These inserts are used by athletes for different reasons. Runners use orthotics to absorb shock at heel contact and to set up the forefoot for push-off. Basketball players wear them to control their forefeet while jumping and running.
The two main types of orthotics are over-the-counter orthotics and custom-made orthotics. To be eligible for custom orthotics, an examination of the foot and ankle will need to be completed. Afterward, both the foot and ankle will need to be casted and fitted for the proper orthotic. When the fitting process is complete, adjustments can be made to make sure everything fits perfectly.
Over the counter orthotics tend to be more popular than custom fit ones. Athletes who have less severe aches and pains in the foot, ankle or lower back area can use the over-the-counter version of orthotics. Unfortunately, over-the-counter orthotics tend to not work in treating severe injuries or ailments. Whenever you suspect you may need an ankle foot orthotic, you should consult with your podiatrist to determine which type of orthotic is right for you.
Relationship of Heel Spurs to Plantar Fasciitis

Plantar heel pain is a widespread problem that affects many people from different backgrounds. It can make life difficult for those who are affected by it. A common issue is plantar fasciitis. Some studies have linked heel spurs to plantar fasciitis. People with type 2 spurs, or posterior calcaneal spurs, seem to have more pain before and after surgery, and their foot function is not as good as those with other types of spurs. Type 2 heel spurs are categorized based on their location and are typically found on the back of the heel, just above the insertion point of the Achilles tendon. They are more likely to cause plantar fasciitis. Type 2 heel spurs are differentiated from type 1 heel spurs, also known as inferior calcaneal spurs. They are found on the undersurface of the heel bone, and type 3 heel spurs, or superior calcaneal spurs, which are found on the upper surface of the heel bone. If you have a heel spur that is causing you pain, it is suggested that you schedule an appointment with a podiatrist to understand what type of heel spur you have and how your pain might be relieved.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Advanced Ankle & Foot Surgeons. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in O'Fallon, and New Baden, IL . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
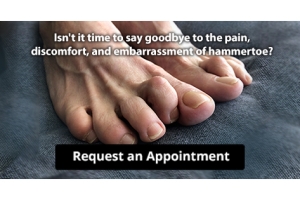
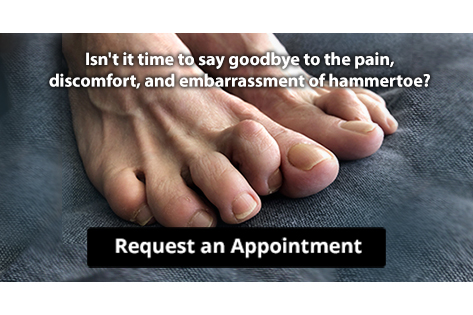
Causes of Hammertoe

Hammertoe, a common foot deformity characterized by an abnormal bending of one or more toes at the middle joint, can develop due to various factors. First, genetics can play a significant role, as individuals with an inherited foot structure that predisposes them to hammertoes may be more susceptible. The choice of footwear is another critical factor, as tight, narrow, or ill-fitting shoes can force the toes into unnatural positions, subjecting the toe joints to excessive pressure. High-heeled shoes, in particular, can push the toes forward into a bent position, contributing to hammertoe development. Additionally, a toe length discrepancy, where one toe is longer than the others, can increase the risk, especially if it consistently rubs against the inside of the shoe. Conditions like arthritis can also lead to joint inflammation and deformities, including hammertoes. Past toe injuries or trauma can disrupt toe joint alignment, and muscle imbalances affecting toe movement can also play a role. If you have developed a hammertoe, it is suggested that you schedule an appointment with a podiatrist for early intervention and treatment to help manage the condition and prevent it from worsening.
Hammertoe
Hammertoes can be a painful condition to live with. For more information, contact one of our podiatrists from Advanced Ankle & Foot Surgeons. Our doctors will answer any of your foot- and ankle-related questions.
Hammertoe is a foot deformity that affects the joints of the second, third, fourth, or fifth toes of your feet. It is a painful foot condition in which these toes curl and arch up, which can often lead to pain when wearing footwear.
Symptoms
- Pain in the affected toes
- Development of corns or calluses due to friction
- Inflammation
- Redness
- Contracture of the toes
Causes
Genetics – People who are genetically predisposed to hammertoe are often more susceptible
Arthritis – Because arthritis affects the joints in your toes, further deformities stemming from arthritis can occur
Trauma – Direct trauma to the toes could potentially lead to hammertoe
Ill-fitting shoes – Undue pressure on the front of the toes from ill-fitting shoes can potentially lead to the development of hammertoe
Treatment
Orthotics – Custom made inserts can be used to help relieve pressure placed on the toes and therefore relieve some of the pain associated with it
Medications – Oral medications such as anti-inflammatories or NSAIDs could be used to treat the pain and inflammation hammertoes causes. Injections of corticosteroids are also sometimes used
Surgery – In more severe cases where the hammertoes have become more rigid, foot surgery is a potential option
If you have any questions please contact our office located in O'Fallon, and New Baden, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Hammertoes?
Hammertoes are painful deformities that frequently form on the second, third, or fourth toe. The condition is often caused by an issue in foot mechanics. This can be caused by the person’s specific gait or the manner in which they walk, or by shoes that do not comfortably fit the deformity. Hammertoes can be formed after wearing shoes that are too narrow or short for the foot or have excessively high heels. Shoes that are not properly sized will force the toes into a bent position for long periods of time. This can cause the muscles to shorten and toes to bend into the deformity of a hammertoe.
Hammertoe can also be caused by complications from rheumatoid arthritis, osteoarthritis, trauma to the foot, heredity, or a cerebral vascular accident. Pain and difficult mobility of the toes, deformities, calluses, and corns are all symptoms of a hammertoe.
Someone who suspects they have the symptoms of a hammertoe should consult with a physician—particularly a podiatrist. Podiatrists diagnose and treat complications of the foot and ankle. If the podiatrist discovers that the affected toes are still flexible, treatment for the hammertoe may simply involve exercise, physical therapy, and better-fitting shoes. Treatment for hammertoes typically involves controlling foot mechanics, such as walking, through the use of customized orthotics.
For more serious cases in which the toes have become inflexible and rigid, surgery may be suggested. During the operation, the toe would receive an incision to relieve pressure on the tendons. A re-alignment of the tendons may then be performed by removing small pieces of bone to straighten the toe. In some cases, the insertion of pins is needed to keep the bones in the proper position as the toe heals. The patient is usually allowed to return home on the same day as the surgery.
If surgery is performed to repair a hammertoe, following the postoperative directions of your doctor is essential. Directions may include several stretches, picking up marbles with your toes, or attempting to crumple a towel placed flat against your feet. Wear shoes that have low heels and a wide amount of toe space to maintain comfort. Closed-toe shoes and high heels should be avoided. Shoes with laces allow the wearer to adjust how fitted he or she may want the shoes to be and also allow for greater comfort. To provide adequate space for your toes, select shoes that have a minimum of one-half inch of space between the tip of your longest toe and the inside of the shoe. This will also relieve pressure on your toes and prevent future hammertoes from forming.
Other preventative measures that can be taken include going shopping for new shoes in the middle of the day. Your feet are its smallest in the morning and swell as the day progresses. Trying on and purchasing new shoes midday will give you the most reliable size. Be sure to check that the shoes you purchase are both the same size. If possible, ask the store to stretch out the shoes at its painful points to allow for optimum comfort.
Managing a Broken Foot

A broken foot, resulting from various causes such as sports injuries, falls, or accidents, can significantly impact your daily life. With 26 delicate bones in each foot, fractures are common and can lead to changes in physical appearance and movement. Symptoms of a broken foot include sudden or gradual pain, difficulty in bearing weight, swelling, bruising, altered gait pattern, and poor balance. Long-term treatment is needed for effective recovery. It typically involves the use of protective casts, boots, or supportive footwear to shield the foot during the healing process. The healing process for bones usually spans six to eight weeks, though the duration may extend based on the severity of your fracture. Beyond immediate care, rehabilitation exercises play an important role in restoring range of motion, mobility, strength, and balance. Because neglecting proper treatment can result in complications, it is imperative to prioritize comprehensive and sustained care for a broken foot. By adhering to these measures, individuals can optimize the healing process, minimize risks, and regain full functionality, ensuring a smoother road to recovery. If you have broken your foot, it is suggested that you schedule an appointment with a podiatrist as quickly as possible for an exam and appropriate treatment methods,
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact one of our podiatrists from Advanced Ankle & Foot Surgeons. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in O'Fallon, and New Baden, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.